- The notion that diet may be able to get rid of or alleviate chronic pain is a very promising idea.
- However, such nutritional interventions may fail to produce significant results for some individuals and cannot ‘cure’ pain.
- To investigate whether a tailored nutrition program has the potential to address chronic pain, MNT tried one program called Revive — a service that offers nutrition and lifestyle interventions based on a person’s DNA.
- Experts who weighed in on the current research say food can significantly influence the underlying factors that contribute to chronic pain, but the outcome may be different for everyone.
When it comes to managing or treating chronic pain — especially after multiple types of medications fail to provide lasting relief— many people turn to lifestyle changes in hopes that such interventions may be able to alleviate some of the symptoms.
It is important to note that while no one diet or nutritional program can cure chronic pain, foods may influence the biological mechanisms that contribute to chronic pain for many people.
Medical News Today spoke to two experts and tested a DNA-based nutrition program to see whether reducing pain via dietary changes is possible.
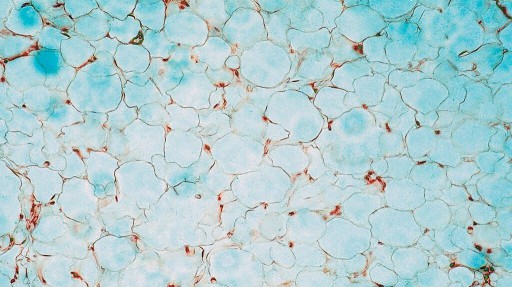
How chronic pain, inflammation, and diet are linked
In that way,
Although there is no one definition for an anti-inflammatory diet, the general recommendation is one that avoids
“Chronic pain often stems from persistent inflammation in the body. This inflammation can be exacerbated or mitigated by dietary choices. Foods high in sugar, unhealthy fats, and certain additives can trigger inflammatory responses, worsening chronic pain. Conversely, adopting an anti-inflammatory diet rich in whole foods and healthy fats can help mitigate inflammation,” she told MNT.
What are some anti-inflammatory foods?
The backbone of an anti-inflammatory diet is foods that are
“For instance, foods rich in omega-3 fatty acids, like fatty fish and nuts, and those high in antioxidants, like berries and leafy greens, can help soothe inflammation, thereby influencing chronic pain. Furthermore, spices such as turmeric and ginger have been recognized for their potent anti-inflammatory properties,” said Costa.
The benefits of including more anti-inflammatory foods in one’s diet may also affect health positively in other ways.
“[It’s] worth noting that these dietary changes don’t just influence pain directly; they also contribute to overall improved health, weight management, and enhanced quality of life, which can indirectly positively impact chronic pain management,” Costa pointed out.
She stressed that as each individual’s body will respond differently to such dietary changes, it is important to follow a tailored approach.
Do ‘DNA-based’ nutrition programs work?
Costa started by explaining
“Epigenetics, essentially the study of changes in organisms caused by modification of gene expression, and DNA-based nutrition programs have the potential to revolutionize dietary guidance,” said Costa. One way this can be achieved is through
“Yet, the science is still maturing and has not reached the point where wholly personalized diets can be accurately developed for individuals based on their genetic makeup alone. Some studies suggest that personalized nutrition advice delivered through digital platforms can prompt more significant and appropriate modifications in dietary behavior than traditional, population-wide advice,” she continued.
Costa underscored that although comprehensive evidence regarding incorporating phenotype or genotype data into personalized nutrition advice is lacking, such data may enhance the effectiveness of these interventions.
She said DNA-based nutrition programs had potential and “may enhance adherence due to their personalized nature,” therefore producing more tangible results for people.
However, she cautioned that they may be just as effective as personalized guidance by a dietitian.
“[The] effectiveness [of DNA-based nutrition programs] may not exceed the benefits of individualized dietary advice grounded in a person’s present diet patterns, medical history, and lifestyle, similar to the guidance provided by a dietitian,” she said.
“While genetics-based nutrition may become a valuable tool in the future, it’s essential to consider all aspects of a person’s health and lifestyle when creating personalized dietary recommendations.”
— Kelsey Costa
Can improving gut health reduce pain?
One such link is a receptor called
“The gut microbiota is a vital intersection between the neuroimmune-endocrine and microbiome-gut-brain axes, potentially impacting chronic pain directly and indirectly. Various signaling molecules from the gut microbiota appear to modulate chronic pain progression by targeting associated receptors and managing peripheral and central sensitization,” explained Costa.
Disrupted gut health: Before or after pain?
“Current evidence mainly says that the chronic pain population shows disturbed gut microbiota compared to the pain-free population. Also, we know already that dietary factors can directly affect gut health,” he told MNT.
Meanwhile, Costa pointed out that an imbalance in gut microbiota has been associated with the worsening of chronic pain disorders, including neuropathic or inflammatory pain, migraines, and fibromyalgia.
She said that the evidence so far suggests that “improving the diversity and balance of gut microbiota may contribute to reducing inflammation and chronic pain,” and hence, such programs targeting gut bacteria with an aim to improve gut health could be helpful.
Still, Dr. Elma said the scientific basis for targeted interventions via the gut microbiome to improve chronic pain was lacking.
Why is treating chronic pain difficult?
When it comes to managing chronic pain, Dr. Elma drew attention to the multifaceted nature of chronic pain and how many factors can influence its frequency and severity, which makes it more complex to treat.
“Chronic pain is multidimensional, and we know that lifestyle factors, including physical activity, sleep, obesity, smoking, alcohol intake, depression, anxiety, and diet, all can play a role in the occurrence, prognosis, and management of pain,” he said.
Dr. Elma singled out diet as a modifiable lifestyle factor that can affect pain in both positive and negative ways.
“Mainly, we need an optimal nutrient intake for general well-being and for a properly functioning nervous system. On the other side, some people might have some allergies or intolerances to specific foods and nutrients, which might trigger certain metabolic responses in the body and contribute to pain processing mechanisms,” he explained.
Not enough research on DNA-based diet plans, yet
Although our understanding of the link between genetics and nutrition is growing, research on DNA-based interventions is still being compiled, gathered, and explored.
“Unfortunately, we are still in the early stages of developing personalized dietary interventions for the chronic pain population due to a lack of robust scientific findings. Most approaches, including DNA-based nutritional interventions, are currently based on hypotheses and proposals,” said Dr. Elma.
“Current DNA kits primarily focus on identifying genetic markers associated with potential responses to certain foods. However, they do not comprehensively assess how an individual’s body responds to specific food ingestion, and they often overlook factors like metabolomics, including gut microbiota responses,” he continued.
Dr. Elma said some people may also have a specific need for certain nutrients compared to the rest of the population due to metabolic differences, highlighting the importance of a tailored intervention.
Another limitation of the research on the link between gut health and pain lies in the nature of the studies conducted.
“There is a lack of interventional studies on the chronic pain population. Current evidence on gut microbiota comes from observational, cross-sectional comparative studies. They compare gut diversity among different populations and deduct associations from these observations. [W]e are lacking studies that target gut microbiota in chronic pain populations with dietary interventions,” said Dr. Elma.
“Overall, I believe that the combination of the developments in artificial data, omics technologies, and increased access to such technologies enable such DNA-based programs to be effectively used in chronic pain populations, considering individual differences,” he added.
Testing the science: My own DNA-based nutrition program for pain
Revive provided the DNA test kit and nutritional counseling service for free. But our opinions, analyses, reviews, or recommendations are ours alone and have not been reviewed, approved, or otherwise endorsed by Revive.
As a Medical News Today editor, I decided to put the science to the test to see if these hypotheses held true in the real world. The U.K.-based service I used is called Revive, which offers individualized solutions for health and well-being — including managing chronic pain, weight loss, long COVID, and blood sugar control.
What the Revive team wanted to achieve with my case was:
- To lower inflammatory signaling from my innate immune system
- To repopulate commensal bacteria and rebuild gut health
- To get advice on medication options and managing chronic pain
My nutrition program for chronic pain was divided into two phases — an immune-resetting diet followed by immunity-building via food.
As part of the preparation for my genetic analysis, I was first sent a DNA test kit.
The DNA test kit
I received the kit in a securely wrapped and padded box via priority post. Inside was a FitBit to keep track of my activity levels, sleep, and heart rate, a charger and extra wrist strap as well as the container to collect my DNA.
By following the informational leaflet that detailed step-by-step instructions, I was able to collect my DNA and post my box back to the company for testing. There was no bloodwork involved, as the DNA was collected via saliva.
Answering the health questionnaire
I first had to answer questions on the healthquiz on their website to give the nutritionist a general idea of my overall health.
The score I received from this questionnaire was calculated and evaluated in five categories: neurological, environmental, exercise, diet, and sleep.
The detailed onboarding health questionnaire also included questions about the current medications I was taking and asked me to describe my chronic pain symptoms and their severity.
The next step was a true/false questionnaire that gave preliminary information about an individual’s likely genetic profile.
Some of the questions included:
- Do you avoid consuming any food and drink because they cause you problems?
- Would you say you have regular bowel movements?
- If applicable, do you have what you class as a normal menstrual cycle? Any concerns to mention?
- Are there any habits or lifestyle changes you want to introduce?
What a diet for chronic pain looks like
The first stage of the nutrition program is usually four weeks. However, as I had international travel planned, the first half of my program was condensed to 21 days.
The nutrition team at Revive said this phase was designed to clear out the digestive system of
The diet involved
The most challenging part of this stage was eliminating many foods and food groups from my diet. I was instructed to cut out all inflammatory foods, such as processed sugar, alcohol, a majority of carbohydrates, dairy, and even nightshade vegetables such as eggplants and tomatoes. My shopping list consisted of organic, grass-fed butter and meats, tofu, miso, cabbage, zucchini, leafy greens, berries, and 90% dark chocolate.
The best part of this diet was that I was allowed to consume a lot of healthy fats — mainly in the form of olive oil and avocado, which are known for their
Probiotics for chronic pain
The second phase of the program involved introducing various prebiotic and probiotic foods and supplements to my diet, which also lasted for another 21 days. Some of the strains of gut bacteria the Revive nutrition team wanted to target, in my case, were Akkermansia muciniphila, and Bifidobacteria.
However, the program I tested did not offer gut microbiome testing to track any of these changes via blood or stool tests, which is an area where the science is very new.
Besides dietary changes, I was also advised to incorporate some well-being practices into my daily routine, such as yoga/breathing practices and grounding exercises.
Sleep was another component I had to keep track of, and I was encouraged to get 7-8 hours of sleep every night.
Did the program ‘cure’ my chronic pain?
In short, no, but neither does Revive claim it will. However, thanks to new nutrition and lifestyle habits I’ve incorporated into my life since being on the program, I have managed to reduce the dosage of my disease-modifying antirheumatic drugs (DMARDs) and experience less frequent episodes of pain.
Since I ended the program, I have not had to use painkillers daily for joint pain. I have only had to use painkillers on four occasions within the last six months.
One big takeaway for me from the program is that when my gut health is disturbed, I tend to experience flare-ups of pain, which serves to show the role of the gut microbiome in pain.